Definition and Key Features
Trauma locking plates are specialized medical devices designed to stabilize fractured bones. Unlike traditional plates, these plates feature a unique locking mechanism that secures screws directly to the plate. This design eliminates the need for the plate to compress against the bone, reducing stress at the bone-implant interface. The rigid fixation provided by trauma locking plates ensures proper alignment of the fracture, even in high-stress areas like the tibial plateau or proximal humerus.
Key features of trauma locking plates include their ability to distribute mechanical loads evenly across the fracture site. This reduces the risk of implant failure and promotes better healing outcomes. The plates also allow for angular stability, which prevents screw loosening and enhances the overall durability of the fixation. These characteristics make them particularly effective for managing complex fractures or fractures in osteoporotic bones.
Types and Materials Used in Trauma Locking Plates
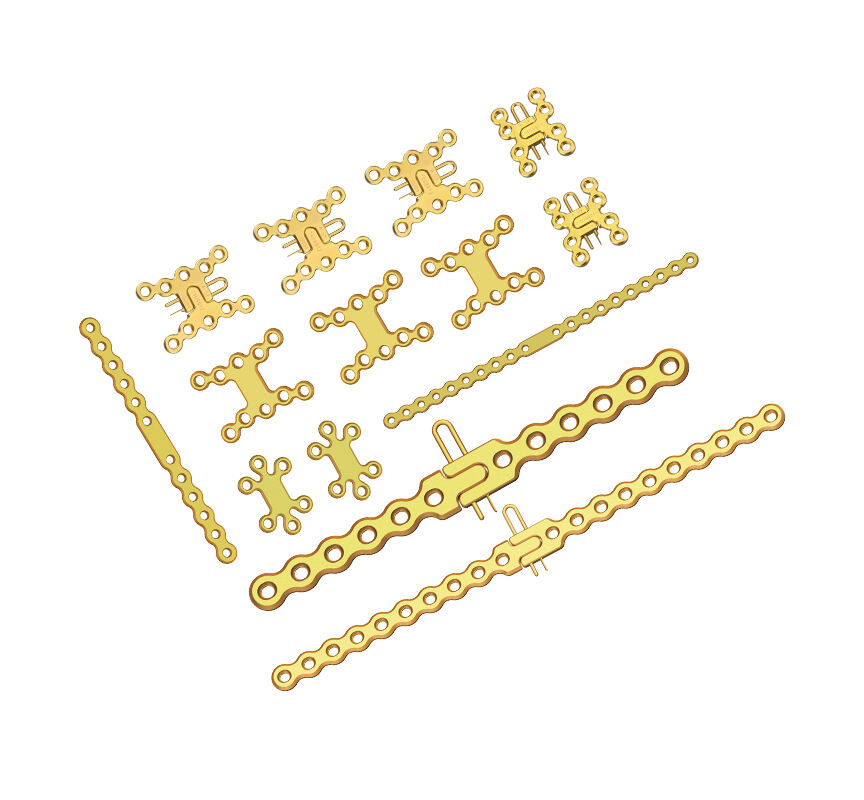
Trauma locking plates come in various types, each tailored to specific anatomical regions and fracture patterns. Common types include proximal humerus plates, distal radius plates, and tibial plateau plates. Each type is designed to address the unique biomechanical demands of the targeted area. For instance, tibial plateau plates are engineered to withstand the high loads experienced in weight-bearing activities.
The materials used in trauma locking plates play a critical role in their performance. Most plates are made from stainless steel or titanium. Stainless steel offers high strength and corrosion resistance, making it suitable for general use. Titanium, on the other hand, is lightweight and biocompatible, reducing the risk of allergic reactions and promoting better integration with the bone. Some plates also feature coatings or surface treatments to enhance their durability and reduce wear over time.
How Trauma Locking Plates Work in High-Stress Fractures
Mechanism of Action
Trauma locking plates function by creating a stable environment for fractured bones to heal. Their unique locking mechanism secures screws directly to the plate, forming a fixed-angle construct. This design eliminates the need for the plate to press against the bone, reducing stress at the bone-implant interface. By doing so, the plates distribute mechanical loads evenly across the fracture site, minimizing the risk of implant failure.
The rigid fixation provided by these plates ensures that fractured bones remain aligned during the healing process. This alignment is critical in high-stress areas, such as the tibial plateau or proximal humerus, where improper healing could lead to long-term complications. The angular stability offered by trauma locking plates prevents screw loosening, even under significant mechanical stress. This feature enhances the durability of the fixation and supports the natural healing process.
Why Trauma Locking Plates Are Ideal for High-Stress Fractures
Trauma locking plates excel in managing high-stress fractures due to their biomechanical advantages. These plates provide superior stability, which is essential for fractures in weight-bearing regions. By maintaining alignment and reducing micromovements at the fracture site, they promote faster and more reliable healing. This makes them particularly effective for treating fractures in athletes or individuals with active lifestyles.
Their ability to handle complex fracture patterns sets them apart from traditional fixation methods. In cases involving comminuted or osteoporotic fractures, trauma locking plates offer a reliable solution. The plates adapt to various anatomical challenges, ensuring proper fixation even in difficult cases. Additionally, their design facilitates early weight-bearing, which accelerates recovery and helps patients regain mobility sooner.
Research highlights the effectiveness of trauma locking plates in reducing the risk of complications. Their rigid fixation minimizes the likelihood of screw pullout or implant failure, even under high stress. This reliability makes them a preferred choice for surgeons managing challenging fractures in demanding anatomical locations.
Benefits of Trauma Locking Plates
Enhanced Stability and Reduced Risk of Implant Failure
Trauma locking plates provide unmatched stability during fracture management. Their unique locking mechanism secures screws firmly to the plate, creating a fixed-angle construct. This design prevents micromovements at the fracture site, which often lead to complications like implant failure. By evenly distributing mechanical loads across the bone, these plates reduce stress on individual screws and the bone-implant interface. This feature ensures that the fixation remains durable, even in high-stress areas such as weight-bearing joints.
The angular stability offered by trauma locking plates minimizes the risk of screw loosening. This is particularly important in cases involving osteoporotic bones, where traditional plates may fail due to poor bone quality. Surgeons rely on these plates to maintain alignment and support throughout the healing process, ensuring better outcomes for patients with complex fractures.
Faster Healing and Early Weight-Bearing
Trauma locking plates accelerate the healing process by creating an optimal environment for bone regeneration. Their rigid fixation keeps fractured bones aligned, allowing natural healing to occur without unnecessary delays. Patients benefit from reduced recovery times, as the plates minimize complications like delayed union or nonunion of fractures.
One of the most significant advantages of these plates is their ability to support early weight-bearing. This feature is crucial for patients recovering from fractures in weight-bearing regions, such as the tibia or femur. Early mobility not only improves physical recovery but also reduces the risk of complications like muscle atrophy or joint stiffness. Athletes and individuals with active lifestyles particularly benefit from this feature, as it allows them to return to their routines more quickly.
Versatility in Treating Complex and Osteoporotic Fractures
Trauma locking plates demonstrate exceptional versatility in managing a wide range of fractures. Their design adapts to various anatomical challenges, making them suitable for treating complex fracture patterns. Surgeons often use these plates in cases involving comminuted fractures, where multiple bone fragments require precise alignment and stabilization.
These plates also excel in managing fractures in osteoporotic bones. The locking mechanism ensures secure fixation, even in bones with reduced density. Traditional plates often struggle in such cases, as poor bone quality increases the risk of screw pullout or implant failure. Trauma locking plates overcome these challenges, providing reliable solutions for elderly patients or those with underlying bone conditions.
Their adaptability extends to different anatomical regions, including the proximal humerus, distal radius, and tibial plateau. Each type of plate is designed to meet the specific biomechanical demands of its target area, ensuring effective treatment for a variety of fracture types. This versatility makes trauma locking plates an indispensable tool in modern orthopedic surgery.
Limitations and Challenges of Trauma Locking Plates
Cost and Accessibility
Trauma locking plates often come with a high price tag. The advanced materials, intricate design, and manufacturing processes contribute to their cost. For many healthcare facilities, especially in low-resource settings, acquiring these plates can strain budgets. Patients without adequate insurance coverage may also face financial challenges when opting for this treatment.
Accessibility remains another concern. In rural or underserved areas, hospitals may lack the necessary inventory of trauma locking plates. Limited access to these devices can delay treatment for patients with complex fractures. Addressing these issues requires collaboration between manufacturers, healthcare providers, and policymakers to ensure equitable distribution and affordability.
Surgical Complexity and Training Requirements
The use of trauma locking plates demands a high level of surgical expertise. Surgeons must understand the biomechanics of the plates and their application in various fracture patterns. Improper placement or technique can compromise the stability of the fixation, leading to suboptimal outcomes.
Training programs for surgeons often emphasize traditional plating methods. Transitioning to trauma locking plates requires additional education and hands-on experience. This learning curve can deter some surgeons from adopting the technology. Healthcare institutions must invest in training initiatives to equip surgeons with the skills needed for successful implementation.
Patient-Specific Factors and Potential Complications
Not all patients are ideal candidates for trauma locking plates. Factors such as bone quality, age, and overall health can influence the success of the procedure. For instance, patients with severe osteoporosis may still face challenges despite the advantages of locking plates. Surgeons must carefully evaluate each case to determine the most appropriate treatment option.
Potential complications, though rare, can occur. These include infection, screw loosening, or irritation at the implant site. In some cases, the rigid fixation provided by the plates may hinder natural bone remodeling. Surgeons must monitor patients closely during the recovery process to address any issues promptly.
Comparison with Other Treatment Options
Traditional Plates
Traditional plates have been a cornerstone in fracture management for decades. These plates rely on compression between the plate and the bone to stabilize fractures. Surgeons often use them for straightforward fractures where minimal stress is placed on the implant. Traditional plates work well in cases where the bone quality is good, and the fracture pattern is simple.
However, their reliance on bone-plate contact can lead to complications. The pressure exerted by traditional plates may compromise blood flow to the bone, slowing the healing process. In high-stress fractures, these plates often fail to provide sufficient stability. Screw loosening and implant failure occur more frequently, especially in osteoporotic bones or weight-bearing regions. Compared to trauma locking plates, traditional plates lack the angular stability needed for complex or high-stress fractures.
External Fixation
External fixation involves stabilizing fractures using a frame or pins placed outside the body. This method is commonly used for open fractures or cases with severe soft tissue damage. External fixators allow surgeons to stabilize the bone without directly exposing the fracture site, reducing the risk of infection in contaminated wounds.
While external fixation offers advantages in specific scenarios, it has limitations. The external frame can be cumbersome for patients, affecting mobility and comfort. Prolonged use may lead to pin-site infections or loosening of the fixator. Additionally, external fixation provides less rigid stability compared to trauma locking plates. For high-stress fractures, this method may not offer the durability required for optimal healing. Trauma locking plates, with their internal fixation and angular stability, often provide a more reliable solution for complex fractures.
Intramedullary Nails
Intramedullary nails are long rods inserted into the bone's medullary canal to stabilize fractures. Surgeons frequently use them for fractures in long bones, such as the femur or tibia. These nails provide strong internal support and allow for early weight-bearing in many cases. Their minimally invasive insertion technique reduces soft tissue disruption, promoting faster recovery.
Despite their benefits, intramedullary nails have drawbacks. They may not be suitable for fractures near joints or in bones with complex anatomy. Misalignment during insertion can lead to complications, such as malunion or rotational deformities. In high-stress fractures, intramedullary nails may not distribute mechanical loads as effectively as trauma locking plates. The locking mechanism of trauma plates ensures superior stability, making them a preferred choice for fractures in challenging locations or under significant stress.
Trauma locking plates have transformed high-stress fracture management by providing unmatched stability and promoting faster recovery. Their adaptability makes them an essential tool for treating complex fractures in challenging cases. While cost and surgical expertise remain obstacles, the advantages often outweigh these concerns. These plates empower healthcare providers to achieve better outcomes by ensuring precise alignment and durable fixation. Comparing trauma locking plates with other treatment methods helps surgeons make informed decisions tailored to each patient’s needs. This understanding enhances the quality of care and supports optimal recovery for individuals with high-stress fractures.
 EN
EN
 FR
FR
 ES
ES
 AR
AR